| Especially in early cases, the detection
of tear film related pathology of the ocular surface during routine clinical eye
examination, is not always easy and straightforward. Therefore, a number of specific tests such as Schirmer Test,
Fluorescein and Rose Bengal Staining, Tear Ferning Test, Conjunctival Impression Cytology,
etc. have usually to be added to the current eye examination to fomulate the correct
diagnosis (Farris 1983, Goren 1988, Rolando 1983b, Rolando 1985).
Unfortunately the adjunct of these
specific tests to the routinely used series of clinical ophthalmologic examinations,
results time expensive and it is often neglected by the general ophthalmologist.
This leads to the consequence that the
diagnosis of tear fllm disorders by the general ophthalmologist is not as frequent as it
could be, with the obvious consequences for the well-being of the patients.
As always in medicine, the basis for a
correct diagnostic approach to a disease are: an intelligent collection of symptoms
(anamnesis) and a careful observation.
While there is a rather standardized way
for collecting the ocular surface signs, the collection of typical symptoms and their
relevance as a diagnostic indicator has not been established yet. The definition of dry
eye as a disorder of the tear film due to tear deficiency or/and tear evaporation which
causes damage to the ocular surface and is associated with symptoms or ocular discomforts,
clearly underlines that in the manifestation of the disease the subjective symptomatology
has a relevant part.
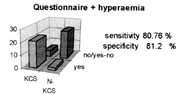
THE DRY EYE QUESTIONNAIRE
We developed a questionnaire based on the
symptoms and the history which are more frequently reported by dry eye patients.
In order to select the three most
frequent and specific symptoms for dry eye, 20 patients with tear film related ocular
surface diseases and 20 patients with non tear film related ocular surface diseases have
been selected. From these patients on the basis of a list of dry eye symptoms present on
the ophthalmic literature (Goren et al 1988) the three symptoms with the best sensitivity
and specificity detecting dry eye among normal eyes and eyes with different eye surface
pathology were selected, and identified as fundamenta/ symptoms, while the
remaining were considered accessory symptoms (table 1).
Our questionnaire, largely derived from
McMonnies questionnaire (Rolando et al 1983b) consisted of five main sections: apart of
the already mentioned fundamental symptoms (section 1) and accessory
(section 2), included fundamental and accessory symptoms time relations, environmental
stress condition related symptoms (section 3), need of topic therapy (section
4), use of systemic drugs (section 5) and presence of systemic diseases (section
6) able to produce or associated with dry eye conditions. Table 2 describes the details of
the questionnaire.
The overall evaluation of the answers can
give a reasonable understanding of the origin of ocular surface disease, but a
quantitative scoring will give more precise information on the level of risk that the
patient has to be primarily affected by a tear film related ocular surface disease.
SCORING SYSTEM
For every symptom considered in the
questionnaire a score is given according to an analogic semi-quantitative presentation,
composed by a line with a ruler graded zero to nine on which the patients, with the help
of a staff member, should mark the entity of his/her symptomatology; in this way a
sub-total score for each symptom was obtained.
The total score for each patient was
calculated by the sum of the single sub-total scores except for the fact that the main
symptoms are scored on the basis of the sum of the sub-lotal scores, while the accessory
symptoms are scored by the sum of the sub-total scores divided by three.
In the sections three to six, each
positive answer to any of the questions scored 1.
The questionnaire was applied to a
population of 268 patients including a group of 112 healthy normals (age = 62+/- 18,
female/male ratio (f/m) = 2.7), a group of 43 ophthalmic patients with no ocular surface
diseases (no-osd) (age = 67±12, f/m =2), a group of 70 non tear film related ocular
surface diseases (osd-no kcs) (age = 53±9, f/m=2.05) and a group of 43 patients with tear
film related ocular surface diseases (kcs) (age = 56±13, f/m = 6.1).
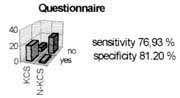
The sensitivity and speciflcity of the
questionnaire as a whole in separating the KCS patients from the other groups were tested.
By means of the study of the area under the ROC (Receiver Operator Characteristics)
curves, the score of 17 was then identified as the one with the best ability in separating
dry eyes from normal and other pathologic eyes.
Figure 1 reports the frequency
distribution of symptoms in the four groups of subjects considered; Table I shows
the sensitivity and specificity of each single symptom in separating dry eyes from the
other groups;

Figure 24-1. Localized hypermia
in the interpalpebral fissure. It reflects the importance of exposure and especially of
tear water evaporation in the build-up of eye surface disease in KCS.
Figure 2 shows the best area under ROC
curve indicating the best compromise specificity and sensitivity, obtained when the
questionnaire total score of 17 was used as a separator between dry eye and non dry eye
patients.

Figure 24-2. Lip like fold of
the bulbar conjunctiva. Its detection is made easy by fluorescein, rose Bengal and
lyssamin green staining of the ocular surface
The use of a systematic approach in
symptoms collections in dry eye is in many ways critical. It is a common clinical
experience that very often the dry eye patients will not designate, if not explicitly
asked the occurrence of a precise symptom, while he will generally complain of eye
discomfort.
A characteristic of dry-eye patients is
the frequent incongruence between the level of ocular surface damage and the
symptomatologic complaint.
There are patients with minimal ocular
surface involvement with high level of complaint in front of a large number of patients
with definite typical conjunctival and corneal damage who do not have a spontaneous
declaration of symptoms except an undefined feeling of discomfort. These patients only if
asked for will tell the presence of specific typical symptoms.
Furthermore many patients if not
precisely asked will mismatch symptoms. Burning and pain and foreign body sensation and
hitching being the more frequently confused.
The ocular surface has receptors for
touch, heat and pain. Subjective symptomatology is the result of activation of these
receptors.
As it has been recognized, symptomatology
is a main point in diagnosis of Keratoconjunctivitis Sicca, which has typical subjective
signs and typical time relation occurrence. Our questionnaire showed an interesting
ability to separate dry eyes from non tear related ocular surface diseases, which will
prove useful in the clinic, especially in controversial cases were the ocular surface
pathology is mixed because of the presence of concurring diseases, or in early cases were
the objective symptomatology is not patent.
Systematic and ordered evaluation of the
prevalence and the significance of a number of subjective symptoms could be of great help
in setting diagnostic networks for many ocular surface diseases. A validated questionnaire
could be a useful tool for population screening for dry eye as well as a useful diagnostic
parameter to be used in the clinic.
TABLE 2
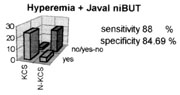
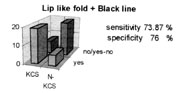
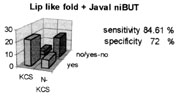
SINGLE TEST
TWO TESTS ASSOCIATED
CLINICAL OBSERVATION
Together with symptoms collection, there
is a number of signs and characteristic aspects of the ocular surface in tear film related
diseases which could be used in a clinical setting as indicators of a tear film problem or
as a hint toward the need of a complete, more complex and time consuming diagnostic
procedure.
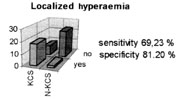
A localized hyperemia confined in the
interpalpebral fissure, the presence of a lip like fold in the inferior conjunctiva, the
irregularity of the black line and a "rapid deteriorating image at Javal
keratometry" are easily collected clinical signs, available to every ophthalmologist
in a routine practice.
LOCALIZED HYPEREMIA
A "conjunctival hyperemia
localized inside the interpalpebral fissure" is a rather frequent presentation of
early tear film related ocular surface patology, when this is not mixed with other more
diffuse surface inflammations
The appearance of interpalpebral fissure
confined hyperemia is a clear suggesting that the protection of the ocular surface, in the
area not already protected by the lids has failed.
The ocular surface protection between
blinks is demanded to the tear film and its failure should consequently implicate that
qualitative or quantitative changes are occurring in the tear film, which impair its
protective function or are at the origin of these localized changes.
Epithelial changes to the interpalpebral
fissure are typical of early Keratoconjunctivitis sicca. The increased tear water
evaporation rate, typical of tear film instability and caused by the consequent
altered spreading or by an inadequate production of the lipid layer, has been reported to
be at the basis of this phenomenon.
When the lacrimal gland secretion cannot
keep the pace with such excessive tear evaporation, both because of an absolute reduction
in tear flow (absolute tear hyposecretion) or because the tear flow, theoretically
sufficient for normal ocular surface needs, cannot satisfy the increased request caused by
environmental conditions, bad blinking habits or contact lens wearing (relative tear
hyposecretion) epithelial changes and inflammation of the exposed ocular surface can
occur. The high rate of water evaporation causes water loss from the tears and increased
electrolyte concentration on the ocular surface, resulting in localized hyper-osmolarity
of the tear film and histologic changes of corneal and conjunctival epithelia.
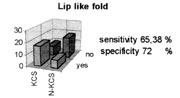
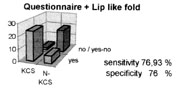
LIP LIKE FOLD OF THE INFERIOR
CONJUNCTIVA
The presence of a "lip like fold
of the inferior conjunctiva" (Rolando et al 1983a) has been suggested to be a
rather sensitive and specific (% sensitivity and % specificity) sign of tear film
related ocular surface problems. It can be recognized by observing the shape of the bulbar
conjunctival layer in correspondence to the inferior lid margin. When present, it can be
recognized as a real fold of the conjunctival sheet in proximity of the inferior tear
meniscus. Such a fold can be just barely visible at the temporal corner, (grade 1),
clearly visible in the temporal bulbar conjunctiva (grade II) or visible also in the
conjunctiva corresponding to the inferior corneal limbus (grade III).
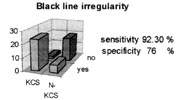
IRREGULARITY OF THE BLACK LINE
The black line (Rolando et al 1990) is an
easily collectable landmark of the tear fluid volume and the evaluation of its morphology
can be used as a diagnostic hint.
When the tear film is colored by means of
a fluorescein strip, under Wood light illumination a distinct black line stands out on the
ocular surface, separating the yellowish precorneal tear film from the adjacent tear
meniscus. Albeit the phenomenon occurs in proximity of both the superior and the inferior
tear menisci usually, the clinical evaluation is made on the inferior black line, which is
easily and instantly examined at the slit lamp. Considering its genesis, the black line
can be considered as a linear area of localized thinning, caused by the traction exerted
on the tear film by the concave thirsty menisci which are originated by the distribution
of the tear fluid in the angle formed by the lid border and the convex surface of the eye.
Up to a certain limit, the thicker are
the tear film and the meniscus, the stronger is the force of traction exerted on the tears
by the meniscus and, as a consequence, the thinner and more regular will be the black
line.
In presence of low volumes of tears and
of a scanty tear meniscus, the centrifugal traction exerted on the tear fluid spread on
the ocular surface will be very low and the black line will appear wider and irregular.
The presence of an irregular black line should be considered a sign of decreased tear
fluid volume available for the ocular surface. The only change needed in the routinely eye
examination is that fluorescein tear staining should be performed before and not after the
instillation of the topical anesthetic during intraocular pressure measurement.
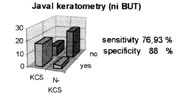
QUALITY OF JAVAL KERATOMETRY
Javal keratometry is based on the reflex
of light from the surface of the precorneal tear film (Gilbard et al 1979). If the
precorneal film because of quantitative or qualitative cannot spread regularly on the
corneal surface or if it has significant thickness irregularities, the light reflex will
result irregular and of low quality, and can be easily detected through the optic system
of the instrument. In a way this is similar to tho functioning of the non invasive
Break-up time (ni-BUT), probably with a lower sensitivity since the ni-BUT explores all
the precorneal surface while the Javal keratometer measure only relatively small areas of
the cornea (approximately 3 mm in diameter) and will be able to detect only tear film
problems occurring in this small central area.
A rapid deterioration of the image at the
Javal keratometry will reflect the rapidity of changes in the quality of vision of the
eyes with tear film problems which are reported to have decreased spatial contrast
sensitivity when compared to normals. Corneal shape irregularities such as keratoconus or
scars, as well as the presence of ulcerations, punctate keratitis, etc. which will affect
the quality of Javal keratometry in dependent or independent way from tear film
distribution and stability should be considered and ruled out.
TESTING THE DIAGNOSTIC POWER OF LOW
TECH TESTS
In order the evaluate the sensitivity and
the specificity of this clinical presentation in the diagnosis of a tear film related
disease, a population of patients with ocular surface disease was evaluated. Such a
population included 26 subjects with diagnosis of KCS assessed on the basis of:
Presence of at least 2 positive results
among
- Schirmer I test < 5.5 mm.
- Typical rose Bengal staining of the ocular
surface (score > 2, by van Bijsterveld's method),
- BUT < 10 seconds, and 25 subjects with
diagnosis of non tear film related ocular surface diseases (n-KCS).
These patients had: typical signs and
symptoms of ocular surface disease but negative results to the dry eye tests:
- Schirmer I test >10 mm.
- No rose Bengal staining of the ocular
surface,
- BUT > 20 seconds.
METHODS
All the patients had to refrain from
using any topical therapy for at least 12 hours before the visit and were evaluated by
means of:
- The use of a symptomatologic questionnaire
(see Table 1) which was considered to be positive for tear film related pathology when
the score was higher than 17 (Gilbard et al 1978).
- The study of the distribution of bulbar
conjunctiva hyperemia, which was considered positive for dry eye diagnosis when it was strictly
localized into the interpalpebral area.
- The research of the presence of a lip
like fold in the inferior bulbar conjunctiva.
- The research of any irregularity of
the black line when observed after fluorescein staining by means of a dry
fluorescein strip in the inferior fornix at dim Wood light.
- The evaluation of the quality of central
pre-corneal tear film surface reflection during Javal keratometry (ni-BUT) (which
was considered positive when irregular targets appeared within 10 seconds after an
unforced complete blink).
- Schirmer I test, rose Bengal staining of
the ocular surface and fluorescein BUT were also performed in every subject and were used
as the gold standard for dry eye diagnosis.
The sensitivity and specificity of the
questionnaire (positive if score >17), of the conjunctival lip like fold, of the
irregularity of the black line and of the observation of tear surface reflection at Javal
Keratometry, alone and in association, in detecting dry eyes ( in respect to the classical
methods used for diagnosis of KCS) were then evaluated.
RESULTS
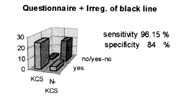
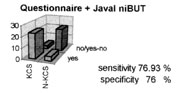
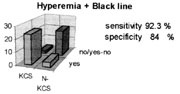
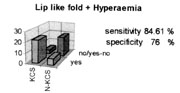
As a single test the presence of irregularity
of the black line had the best compromis between sensitivity and specificity (92%
sensitivity and 76% specificity) in diagnosing dry eye conditions. Among the possible
associations of clinical presentations, the associations Questionnaire +
Irregularity of the black line and Localized hyperemia + Irregularity of the
black line show the best compromise between sensitivity and specificity in
diagnosing dry eye conditions.
Dry eye diagnosis is the result of a
composite approach to history, subjective and objective symptomatology of the patient and
is often reached after a quite complex, time consuming sequence of tests.
Easy and quick to be performed tests are
loved by ophthalmologists and patients and have more chances to be used.
Low cost tests, easy to perform during a
routine eye examination such as dry eye questionnaire (Gilbard et al 1978, 1984),
research of a lip like fold at 6 o´clock, research of hyperemia
localized into the interpalpetral area, research of black line irregularity and
irregular targets at Javal keratometry (ni-BUT) have a nice sensitivity and
specificity in diagnosing dry eye conditions.
They are easily learned and mastered by
any ophthalmologist, their use will add no substantial extra time to the examination
schedule and can provide further information about tear film and ocular surface
conditions.
Unfortunately no single test has the
ability of providing a sure diagnosis of dry eye, but can suggest the need of further
investigation and when necessary, in suspect cases, the diagnosis of KCS should be
assessed by performing the classical dry eye tests. |